Neonatal Research in Newcastle-upon-Tyne: standing on the shoulders of giants
Newcastle has made major contributions to neonatal research that have changed the way babies are cared for worldwide
Paediatrics and Child Health has a proud and illustrious history of Neonatal Research in the North East of England, based around the hospitals in Newcastle. The original infirmary in Newcastle was located on Forth Banks and dates back to 1752. It rapidly outgrew the facilities and the current Royal Victoria Infirmary was built and opened in 1906 on the Leazes site in Newcastle. A Lying-In hospital for women existed on a separate site in Newcastle, and maternity services were then moved to the Princess Mary Maternity Hospital opened in the 1920s.
Sir James Calvert Spence was the first full-time Professor of Child Health in England, and the chair is still named in his honour. A full history of Spence is available elsewhere but his philosophy was integral to the development of neonatal care and much of his work was based around The Babies Hospital located on Leazes Terrace in the 1920s-1940s. Spence was the first physician to encourage mothers to stay with their children in hospital as a routine, and emphasised the importance of the family in all aspects of child health - perhaps one of the earliest descriptions of Family Integrated Care (FIC). Spence highlighted the importance of early life social and environmental factors in determining the early origins and health and disease, decades before the discipline of "Developmental Origins of Health and Disease (DOHaD)" came to the fore. There are reports from Spence in 1925 of caring for infants with malnutrition which was associated with over 50% of all hospital admissions in children, many of whom he treated with "...a plentiful daily supply of human milk from known and certified sources' - quite possibly one of the earliest reports of donor human milk!
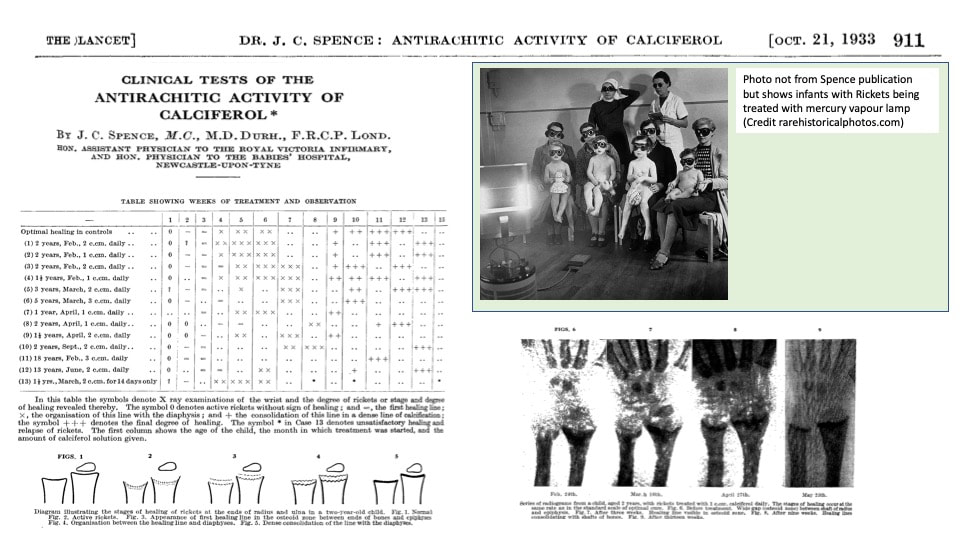
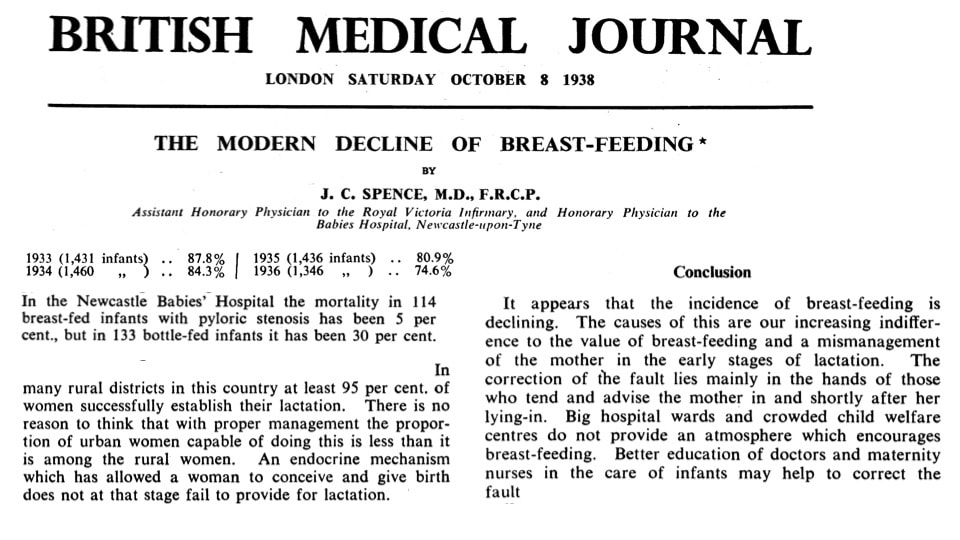
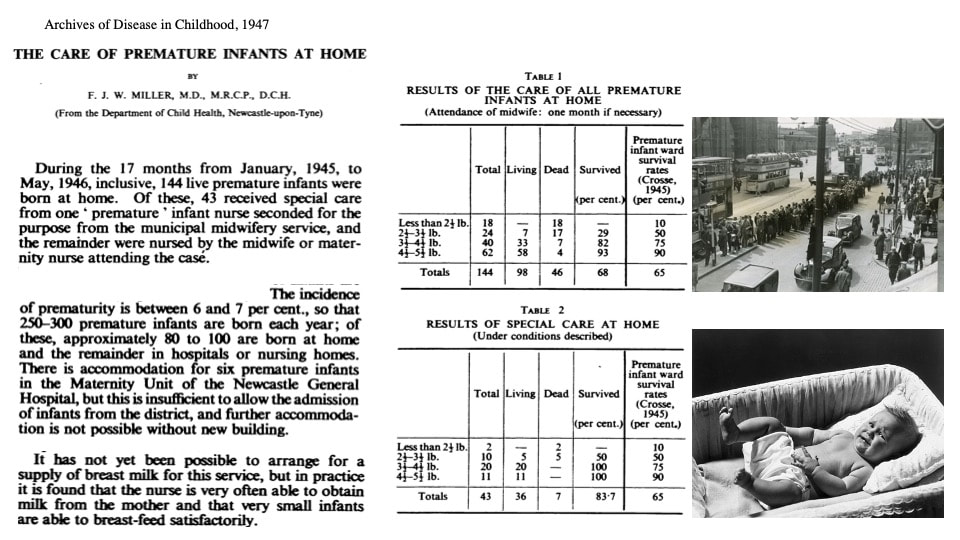
'The Babies Hospital and Mothercraft Centre' was established in 1925 and was used for the 'open air' treatment of rickets due to Vitamin D deficiency which was common place in infants under 12 months, but Spence also set aside rooms for supporting mothers to breast feed. In 1930, Spence described nutritional xerophthalmia and night-time blindness in infants and children due to a lack of dietary vitamin A, and he conducted numerous surveys in the 1930s highlighting the importance of early life nutrition. Spence conducted some of the first studies of treating rickets with calciferol (Vitamin D). Spence had mentored Fred Miller who along with Donald Court became key figures in Newcastle child health. Spence and Miller recognised in the 1930s an alarmingly high rate of infant mortality (91 per 1000 infants died) around twice the rate of the more affluent south of England. In 1937 (the year King George VI rose to the throne, Neville Chamberlain was Prime Minister and the 999 emergency phone number was first introduced) Spence and Miller reported that the major causes of childhood mortality were prematurity and infections, but World War II intervened before further study could be commenced.
The Babies Hospital started life as the 'West End Nursery' (1914-1924) located on Westmoreland Road near to the Tyne river, which provided care for babies of women working in the local munitions factories during WWI. It slowly evolved into a 'Babies Hospital and Mothercraft Centre' to assist with newborn feeding difficulties and was re-located to Leazes Terrace (on the other side of Leazes Park from the current Infirmary) opening in 1925. During WWII the Babies Hospital was re-located out of Newcastle to Blagdon Hall (1940-1948), was formally amalgamated with the Royal Victoria Infirmary in 1944 but continued to provide care at the Leazes site until around 1973 when it was closed.
Developments in the fields of obstetrics emerged in parallel with neonatal medicine. Newcastle had long been recognised as a key site for innovation; as early as 1935 Farquhar Murray had developed the obstetric flying squads (see picture below of woman being treated in a backstreet in Newcastle and watch free film here - great film, no sound, of team arriving in a Bentley and sharing a cigarette after successful blood transfusion for PPH!) and this was further developed by Frank Stabler (perhaps caught on film having the post-event cigarette) in the 1940s. All of this was part of the Newcastle approach and philosophy of shared clinical networks based around the PMMH. In the 1960s and 1970s Newcastle became a leading academic centre funded by the Medical Research Council and recognised globally for work into placental function, maternal physiology and the care of mothers and infants with Rhesus Haemolytic Disease. This was based at PMMH in Newcastle, and many key developments in research and clinical care emerged.
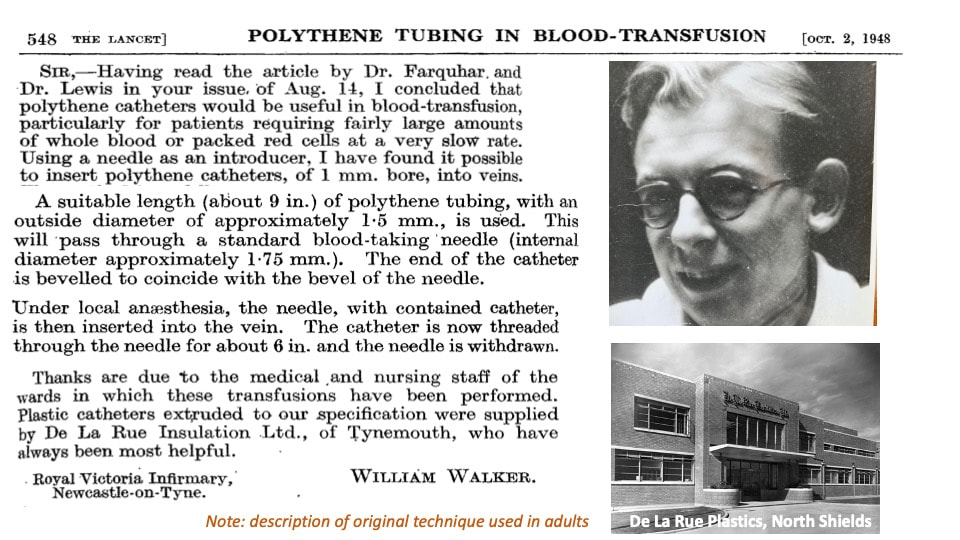
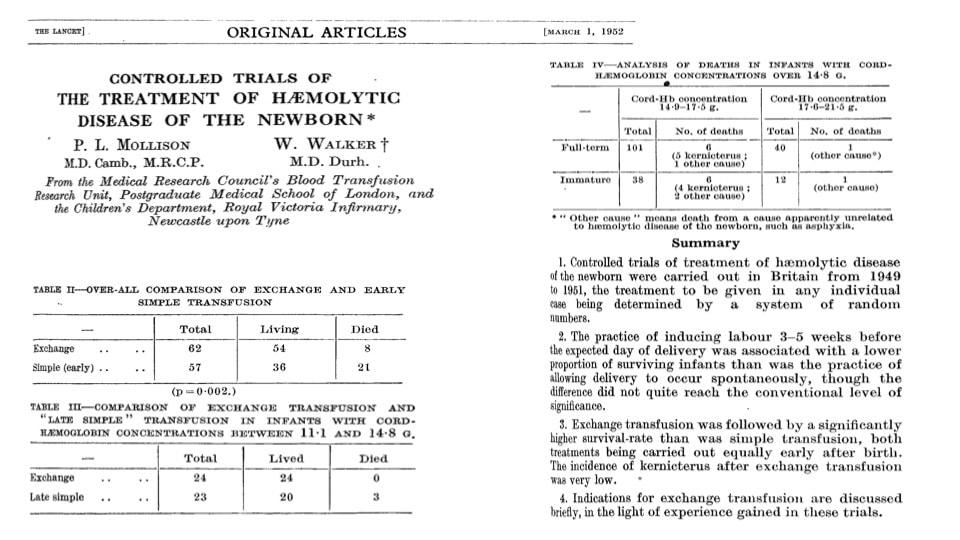
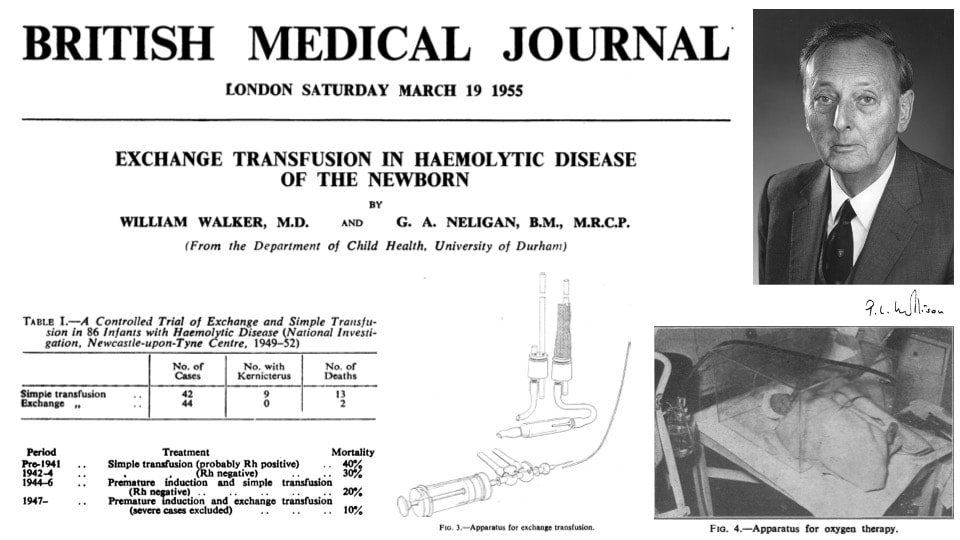
Newcastle emerged as one of the leading centres into the treatment of Rhesus haemolytic disease which was a major contributor to perinatal mortality until maternal injection of anti-Rho D rhesus immunoglobulin (RHIG) in the mid- and late-1960s. Exchange transfusion was first described in the late 1940s, and was used widely between 1950s-1980s but pioneering work into the pathophysiology was conducted by Dr Willie Walker (a paediatric haematologist) who moved to work with Spence in Newcastle after WWII. Specialised umbilical catheters or PICC 'long lines' did not exist back then, however in 1948 Walker describes using the plastic outside of electrical wire from a local factory to create a catheter he could then thread through a wide-bore needle. He describes the technique in an adult (Lancet 1948) but undoubtedly refined the technique for use in newborn infants.
Walker's studies helped lead the way to the development of RHIG but he will be best remembered for refining the technique of exchange transfusion which had first been suggested by Diamond in 1947 to be performed via the umbilical vein. Walker (along with Pat Mollison) conducted meticulous controlled trials between 1949-1952 that proved the success of the technique. His strong support for the need to prove medical interventions using RCTs came some 30 years before Archie Cochrane initiated the collaboration to which his name rightfully endures. Outcomes in Newcastle were better than any other part of the UK leading the Chief Medical Office of the time (Sir John Charles) to allow Walker access to national data on all rhesus-haemolytic deaths so as to improve outcomes across the UK. Walker performed exchange transfusion on hundreds of Newcastle babies in the 1950s and 1960s, undoubtedly saving many lives.
Spence and others created one of the first early life cohort studies - the Thousand Families Study which recruited all 1142 babies born to Newcastle resident mothers in May and June 1947. A red spot was placed on their GP records and they subsequently became known as 'red spot babies': these individuals have been followed up to the present day and form the basis of numerous high impact publications that explore links between early life growth, nutrition and social factors, and health and disease outcomes in later life.
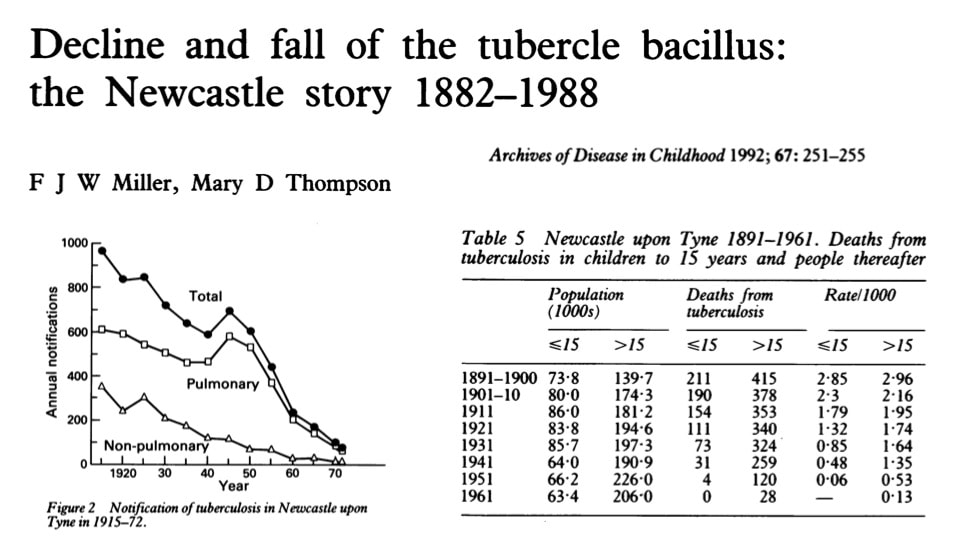
Miller went on to become perhaps one of the first 'neonatologist' in Newcastle being appointed as paediatrician to Newcastle General Hospital in the 1940s and 1950s. In the 1950s, neonatal medicine started to establish as a 'new' sub-specialty and Miller and Neligan led the way in Newcastle. Miller was also famous for his work on Tuberculosis (TB): in the 1940s TB was responsible for 15% of all deaths in children (more than any other single cause) and more than twice that in other parts of the country. Fred Miller's work with others in promoting school immunisation was pivotal in virtually eradicating those deaths.
I
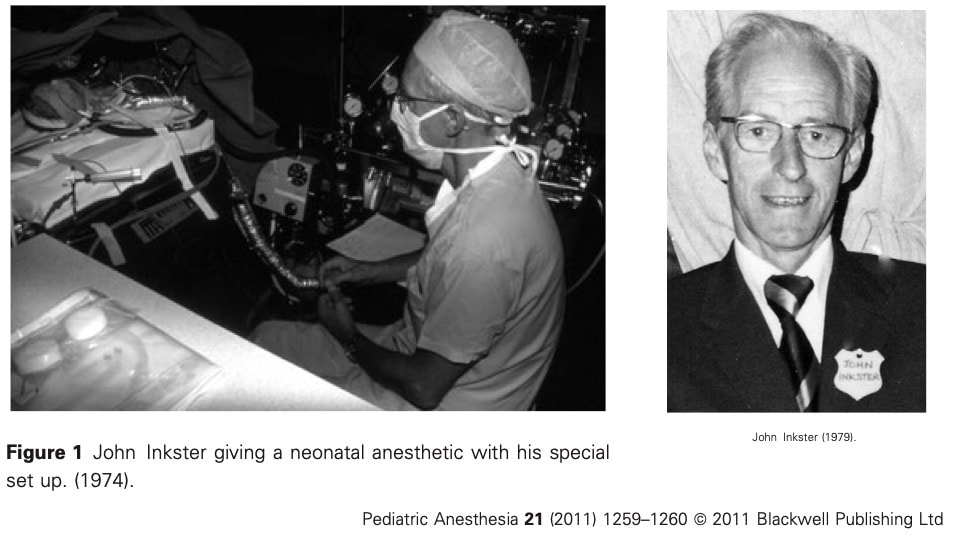
Neonatal surgery emerged in the 1960s and 1970s but required specialised anaesthesia developed out of the skills developed in the Babies Hospital and the Fleming Hospital from the 1930s onwards. Dr John Inkster was a consultant anaesthetist who developed a new technique involving adding resistance during infant expiration, limiting airways collapse and maintenance of Functional Residual Capacity (FRC). Inkster presented this technique to the World Congress of Anaesthesia in 1968 and thereafter 'Positive End Expiratory Pressure (PEEP)' was introduced worldwide and extended to adults.
Remarkably, Inkster himself was born prematurely at 900g along with his twin sister, and his mother (a trained nurse at Great Ormond Street) took them to be cared for at home perhaps demonstrating that early discharge really is beneficial! At the Fleming, Inkster pioneered new approaches particularly focusing on the importance of minimising dead space in neonates using small tubes and connectors. Inkster's advances undoubtedly saved many lives and his collaborations with Hey and others were pivotal in improving neonatal outcomes.
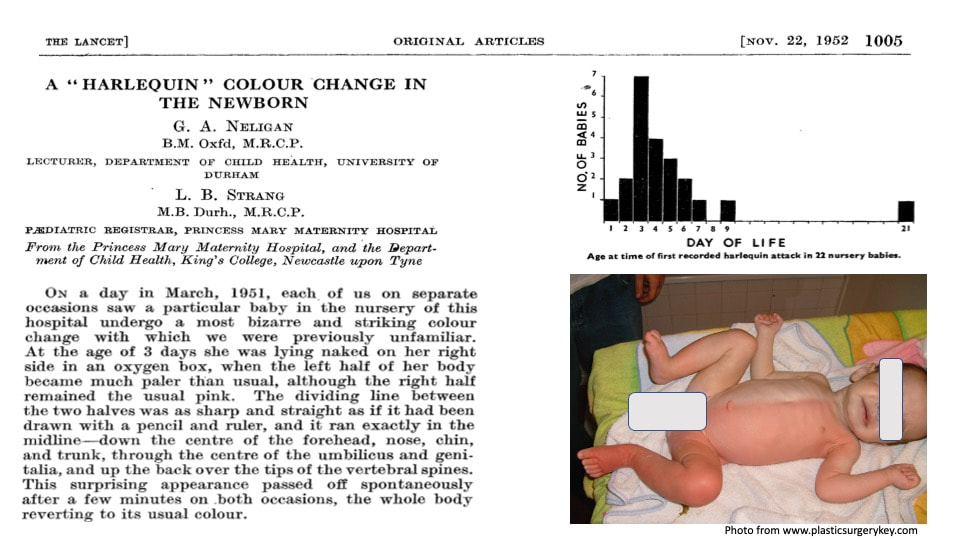
Gerald Neligan (1918-1976) was a key figure in paediatrics in Newcastle from 1950, and although he was appointed to undertake general paediatrics at the RVI, he spent most of his time on the neonatal unit at PMMH. He was an exacting clinician and had high expectations of his residents. Professor Donald Court (who followed James Spence as chair) was said to have remarked to trainees that "If you survive the first two months, you will cope with the rest of life". Neligan worked with Prudham and Steiner to document longer term outcomes of survivors until school age (published as The Formative Years, 1974), and Neligan worked with members of the MRC unit in Aberdeen to construct some of the first centile curves for birthweight and gestation. Neligan was an observant clinician and is credited with the first published description of harlequin colour change in the newborn. Importantly, Neligan describes that the nursing staff had already noticed this, showing all paediatricians that they should always listen to the nurses! The colour changes were somewhat drastically referred to as 'attacks' that only lasted for a short while, but if '.....instead the baby is simply turned, the attack is brought to an end in a quarter of a minute.... these effects mean [that] we have so far failed to obtain one [photo] good enough for reproduction in black and white. Despite the lack of proof, they still managed a publication in the Lancet! Neligan suggested the attacks were of no pathological significance but that the distribution suggests a temporary imbalance in the central nervous system (possibly in the hypothalamus).
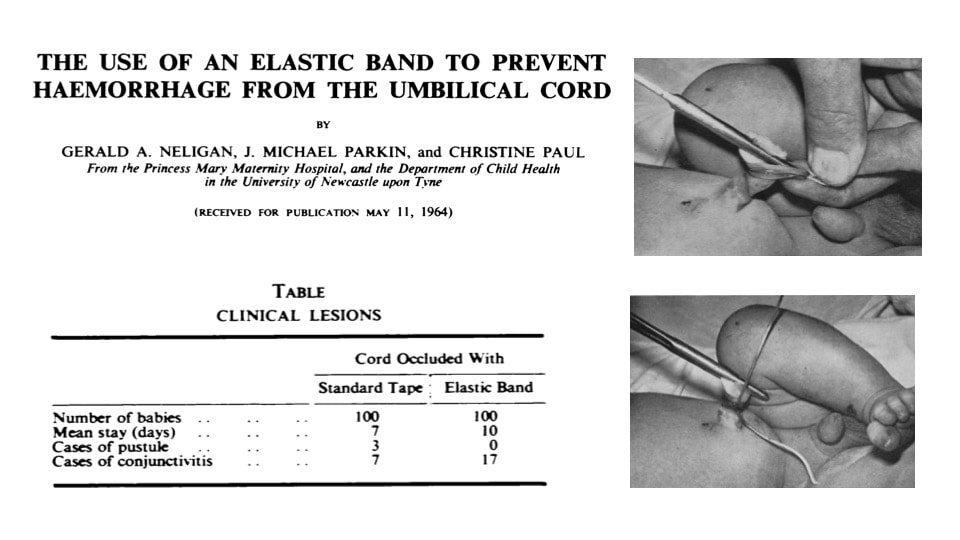
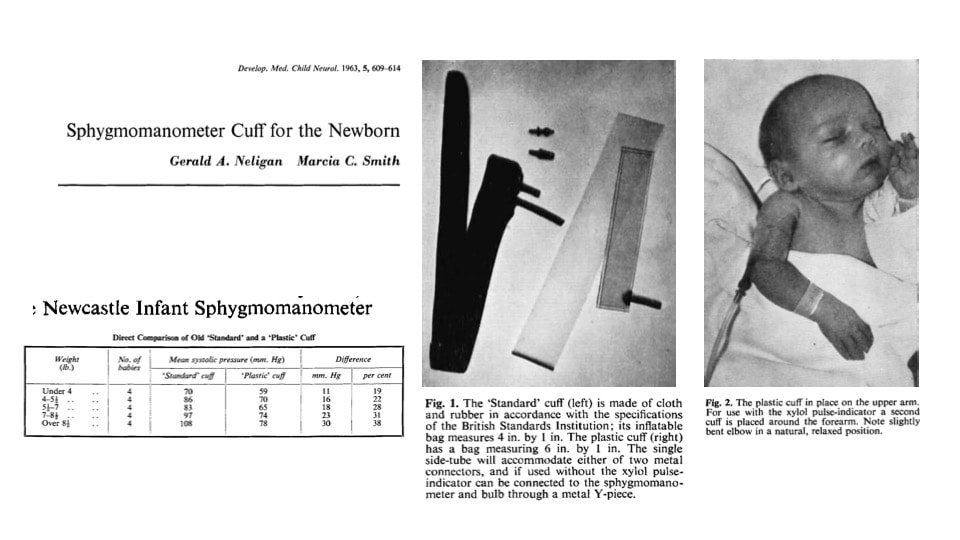
In the late 1950s and 1960s, Newcastle was extremely active in neonatal research. Key figures included Gerald Neligan, Cyril Noble, Mike Parkin, Hans Steiner and many more. Their research included basic physiology, but also clinical practice for example accurate blood pressure measurement. Back then, babies would still die from haemorrhage from the umbilical cord due to misplaced or inadequate cord clamps, and Neligan described using rubber bands to tie the cord. However, it seems the rubber band idea never really took off.
In the 1960s key physiologists (McCance, Dawes, Cross and others working in London, Oxford and Cambridge) conducted basic scientific studies and started to regularly interact with clinicians such as Reynolds, Hey and many others. The death of President Kennedy's son in 1963 from Hyaline Membrane Disease brought world-wide attention to the complications of prematurity and in the UK, Bristol under Peter Dunn started to explore ventilatory support and create Special Care Baby Units for the first time. Reports of 'prolonged' intubation and ventilation started to appear in the mid-1960s, along with use of CPAP which became increasingly common in the early 1970s, and these techniques were particularly developed by Reynolds and teams in London. Surfactant deficiency was a major challenge, but these challenges also led to the development of micro-methods to measure blood cases using capillary and small syringe.
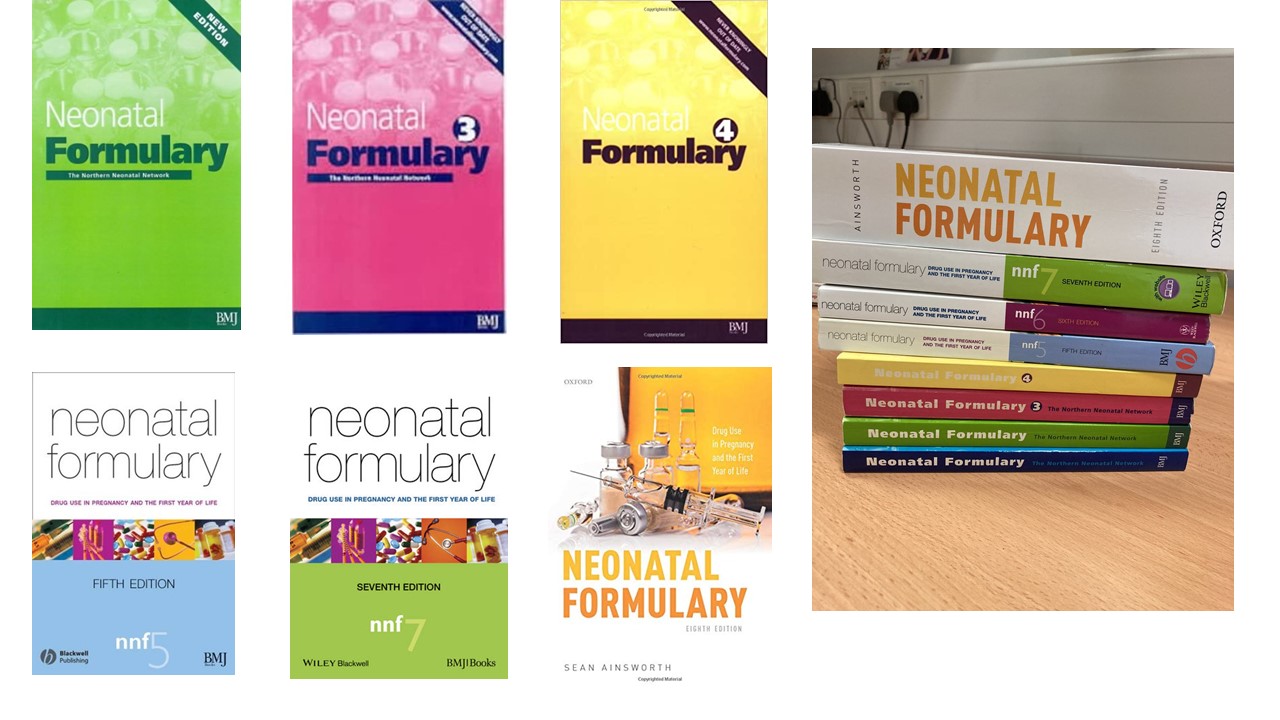
During the 1960s and 1970s, neonatal care in Newcastle was provided at a number of locations including the Newcastle General Hospital (NGH), the Princess Mary Maternity Hospital (PMMH, opened 1923) and the Fleming Hospital which provided paediatric surgery from the 1970s to 1980s. Inkster, along with Dr Edmund Hey (see below) carefully described the use of drugs necessary for neonatal anaesthesia and created one of the first neonatal drug formularies in 1978. This was regularly revised in the 1980s and 1990s, and finally published in 1996. The Neonatal Formulary is regularly updated (now in it's 8th edition and edited by Dr Sean Ainsworth, a former mentee of Hey) and is recognised globally as the authoritative text on drug use in neonates.
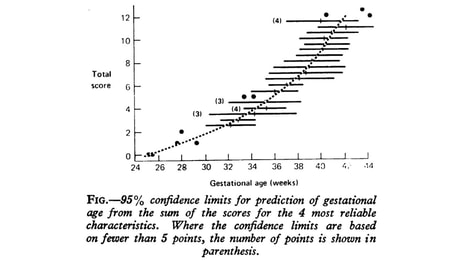
Dr Edmund Hey was appointed to PMMH in 1970s, having trained as paediatric registrar in Newcastle and London. He conducted seminal work with Katz into thermoregulation in newborn infants which led to the worldwide use of double-walled neonatal incubators. Hey was a true pioneer and changed the face of neonatal medicine and research worldwide conducting research into almost every aspect of neonatal medicine. In 1976, along with Professor Mike Parkin, they described the use of the "Parkin score", a simple scoring system based on skin colour and texture, breast development and ear firmness that accurately predicted gestation at birth. It is important to remember that in the 1970s pregnancies were not routinely scanned, and estimations of gestations were often incorrect. Hey also collaborated with Elsie Widdowson from Cambridge, widely recognised as the most influential scientist in neonatal nutrition, and together they published on Fetal Growth and Body Composition (Perinatal Nutrition, 1988).
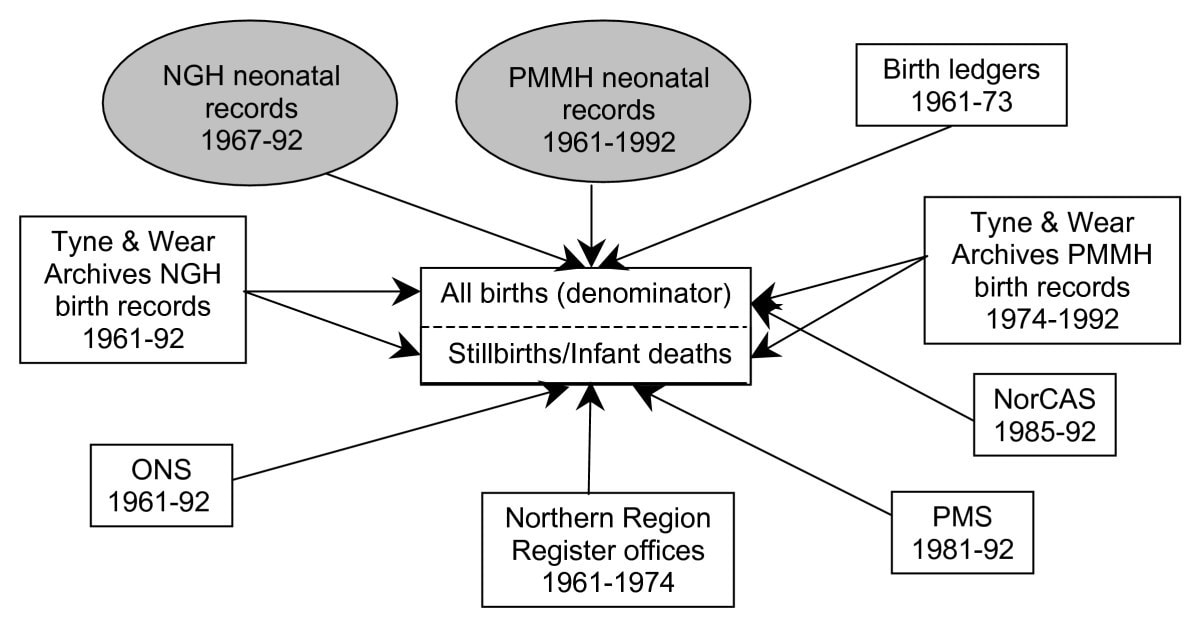
It is difficult nowadays to appreciate the breadth of Hey's interests and achievements for he was a very quiet and un-assuming person who avoided the limelight and disliked speaking in public. Hence, he almost never presented at conferences, or held office bearer status in learned societies, but he was known and respected globally as perhaps the 'eminence grey' of UK neonatology, constantly working and influencing behind the scenes. Those who were lucky to work for him held him in the highest regard. Hey helped develop some of the first ever population based surveys of perinatal mortality and congenital anomaly, both forerunners of national systems of data collection and housed in the Regional Maternity Survey Office (RMSO). In 1984 with support from the regional health authority, Hey established the Fetal Abnormality Survey (later to become NorCAS - northern region congenital abnormality survey) a voluntary collaborative survey and almost certainly the most comprehensive such survey worldwide. Widespread support came from obstetrics, paediatrics and surgery, as well as from paediatricians developing genetics as sub-specialty including Professor Sir John Burn. The RMSO and perinatal epidemiology were further developed by Professor Judith Rankin and Martin Ward Platt in the 1990s. Further surveys based around maternal diabetes, multiple pregnancy and cerebral palsy (established by Professor Alan Colver) emerged out of these collaborations and led to numerous high impact publications.
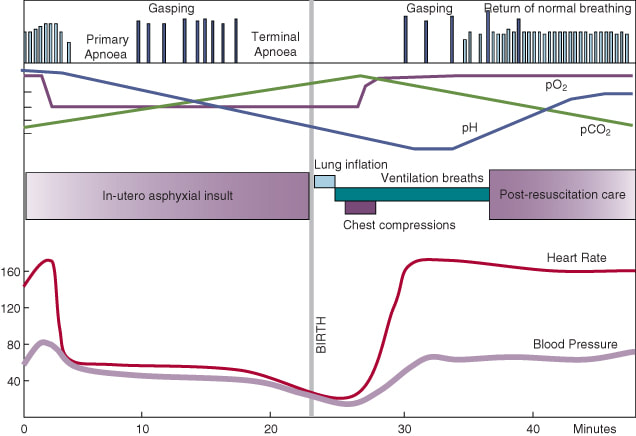
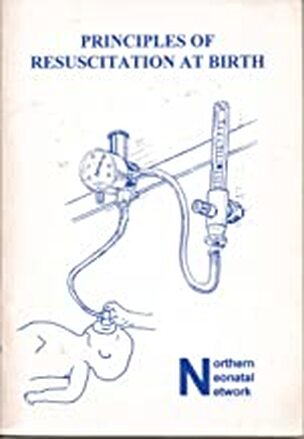
Hey had carefully described newborn adaptation after birth, and response to resuscitative measures. Hey had worked with Kenneth Cross in London in the 1960s before coming to Newcastle and was involved in much of the original research into the physiology of neonatal asphyxia. (Cross was awarded the Sir James Spence medal in 1979 for his contributions to neonatal research and formed the Neonatal Society in 1959, the world's oldest learned society for the promotion of neonatal science.) Hey's work emphasised importance of thermoregulation, airway manoeuvres and response to mask inflation were emphasised and taught to generations of paediatric trainees in the 1970s and further developed with the appointment of Dr David Milligan to NGH in the 1980s. The first booklet written to help midwives, nurses and doctors first appeared in 1980. This teaching programme and booklet became the forerunner of Newborn Life Support (NLS) now taught globally and was developed by Dr Jonathan Wyllie, Sam Richmond and others who had trained under Hey. Wyllie later became the first paediatrician to chair the International Liaison Committee on Resuscitation (ILCOR).
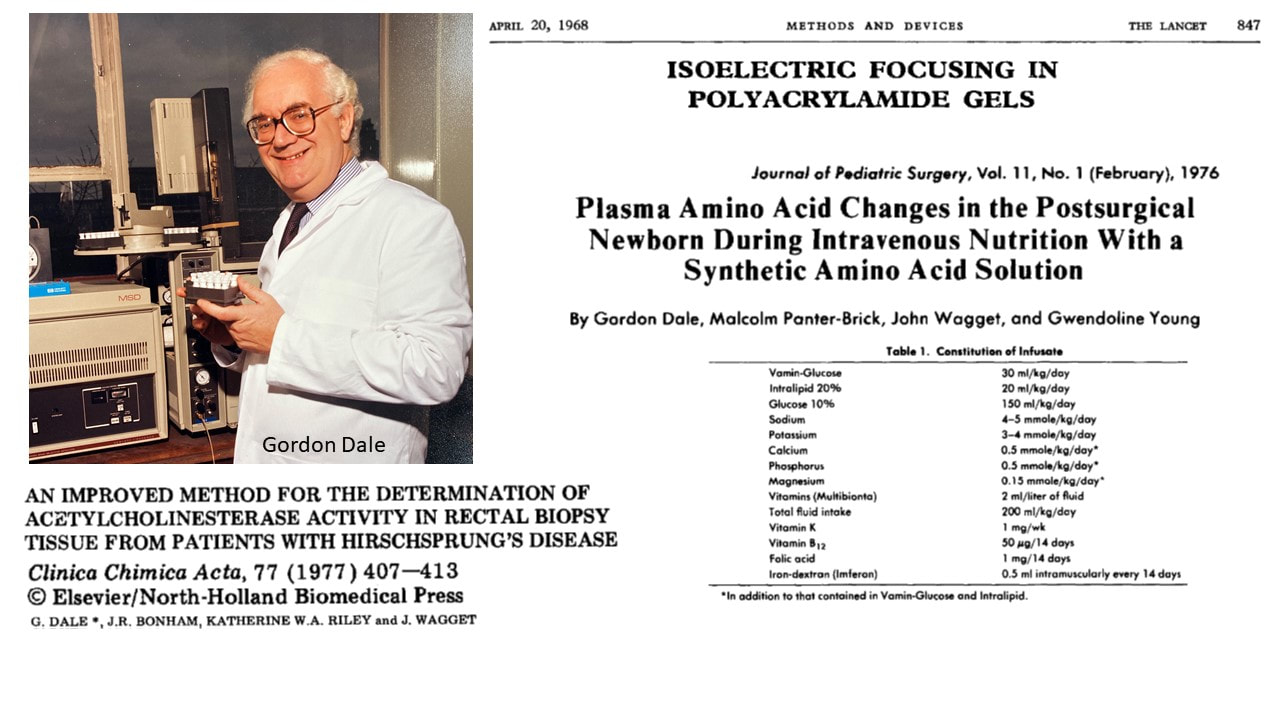
Neonatal medicine and surgery advanced in parallel with many other developments in biochemical and other specialties. Gordon Dale was a biochemical expert, trained in Newcastle who helped refine the technique of iso-electric focusing (now used worldwide) publishing a landmark paper in 1968. Parenteral nutrition was first described in neonates in the mid 1960s, but early solutions based on hydrolysates were extremely problematic until they were replaced by crystalline amino acid solutions. Dale had particular expertise in amino acid profiles and regularly supported the use of parenteral nutrition at the Fleming hospital, as well as helping develop the process of newborn bloodspot screening and developing techniques to provide a more accurate diagnosis of Hirschsprung's disease by staining for acetly cholinesterase in biopsy specimens.
|
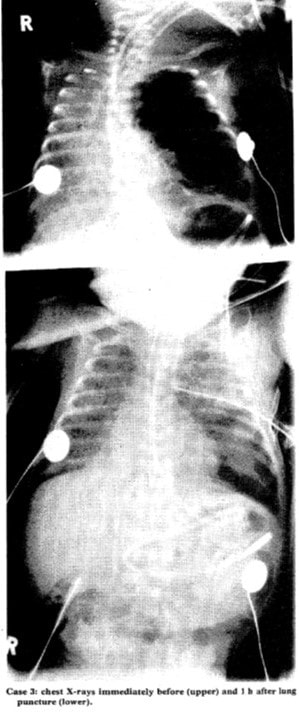
David Milligan conducted key research into failure of cerebral autoregulation and intra-ventricular haemorrhage (Lancet 1980), whilst working as a research fellow at the Hospital for Sick Children in Toronto, having also worked with Kenneth Cross in London in the late 1970s, and been part of Osmund Reynold's group first describing the use of ultrasound to scan the neonatal brain. Osmund Reynolds' and group were probably the pioneers of caring for extremely low birthweight babies in the 1970s. Milligan was appointed as neonatologist/paediatrician to the Newcastle General Hospital (on the other side of the city from the PMMH) in 1982 when there were only 4 intensive care cots, but developed the service with Dr Phil Kenna, rapidly expanded to 12 intensive care cots and established a database, published the first annual report, established regular morning teaching and neonatal follow up - all key developments that continue to this day. Respiratory pathology and treatment were very different in the pre-antenatal steroid and pre-surfactant era and many babies died from complications associated with Pulmonary Interstitial Emphysema (PIE). In 1984 Milligan (along with his mentor Os Reynolds from UCL, London) described the treatment of severe, primarily unilateral PIE by deliberately puncturing large bullae (and thereby creating a pneumothorax which could be drained) to allow lung re-inflation (Lancet 1984). Lung pathology of this type and severity is never seen nowadays.
|
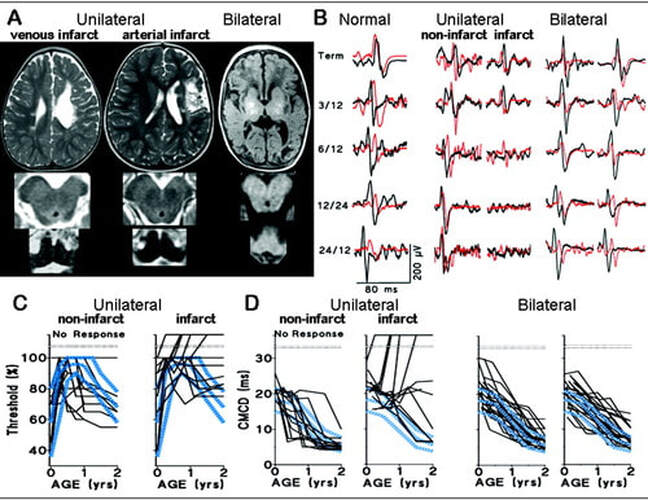
In 1983/84 there was increasing recognition of the need for regional collaboration and a central phone line (the 'Hot Line') was established, one of the earliest examples of a managed clinical network for neonatal care. Regular cerebral ultrasound scanning was established in 1984, neonatal follow up until 2 years of age were included in annual reports from 1985 and a neonatal neurology research centre (first housed in a portacabin) was established at NGH under Prof Janet Eyre who was awarded the Guthrie Medal by the RCPCH in 1990 for her research. These academic/clinical collaborations led to seminal research describing development of the cortico-spinal tracts in infancy and with Prof Al Aynsley-Green, Eyre undertook key research into brain responses to hypoglycemia. 1986 saw the use of High Frequency Oscillatory Ventilation (HFOV) and regular cardiac echo in preterm infants supported by key developments in cardiac scanning led by Dr Stewart Hunter and Dr Chris Wren. Stewart Hunter and colleagues had helped pioneer the use of ultrasound for cardiac examination; he wrote several papers on the use of cardiac ultrasound in the 1970s and laid the foundations for the currently used nomenclature for congenital heart disease. Stewart Hunter worked with Bill Dunlop, Steve Robson and others from the PMMH to publish world leading research on maternal cardiac physiology and cardiac output during labour. Majd Abu-Harb, Sam Richmond, Ed Hey, Chris Wren, Jonathan Wyllie, John Madar and Jon Skinner and others conducted numerous echocardiographic studies and population based research studies on presentation of congenital heart disease in infancy that remain widely cited to the current day.
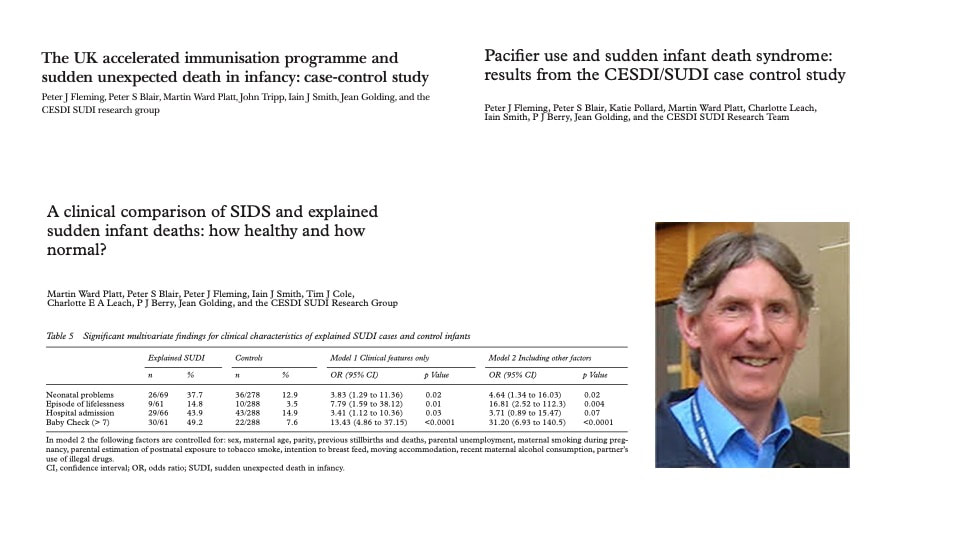
Dr Martin Ward Platt was appointed as neonatologist to the PMMH in 1990 and was heavily involved in extending the regional surveys at the RMSO onto a national agenda. He was key in the development of the Confidential Enquiry into Stillbirth and Death in Infancy (CESDI), and undertook ground breaking studies in relation to Sudden Unexpected Death in Infancy (SUDI) along with Blair and Fleming (from Bristol) whose work in relation to co-sleeping as a risk factor influenced international guidelines for the prevention of 'cot death'. Martin Ward Platt also worked with Professor Sir Al Aynsley-Green, Jane Hawdon and Sanjeev Deshpande to carefully describe patterns of metabolic adaptation for preterm and term infants in the first week of life, determining the importance of ketone bodies in term infants (and their lack in preterm infants) and the importance of breastfeeding to enhance ketogenic ability. Martin Ward Platt was for many years editor and senior editor for the Archives of Disease in Childhood, recognised globally at the highest impact journal for fetal and neonatal research. Before his untimely death in 2019, Martin had supported numerous research projects, postgraduate and masters students and had an encyclopaedic knowledge of published neonatal research.
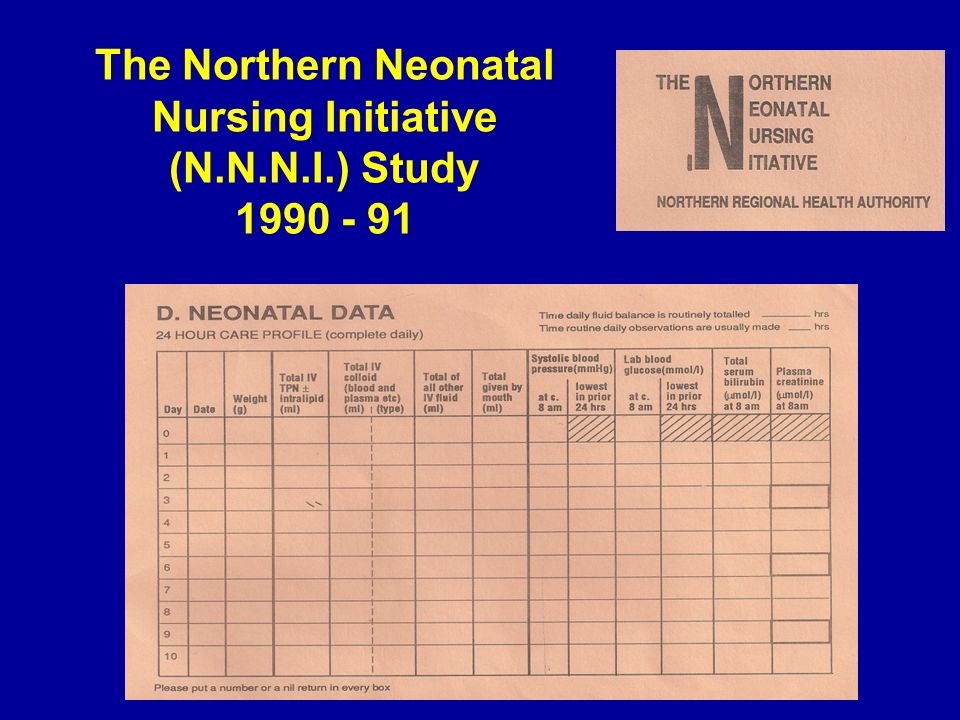
Edmund Hey, Martin Ward Platt and colleagues espoused the importance of collaborative working especially for neonatal research, and Hey rarely took credit for much of the research he initiated. Along with Dr Sam Richmond, David Milligan, Sue Fritz and Win Tin a series of studies were conducted under the auspices of the Northern Neonatal Nursing Initiative (NNNI), perhaps one of the earliest examples highlighting the importance of neonatal nurses in clinical research.
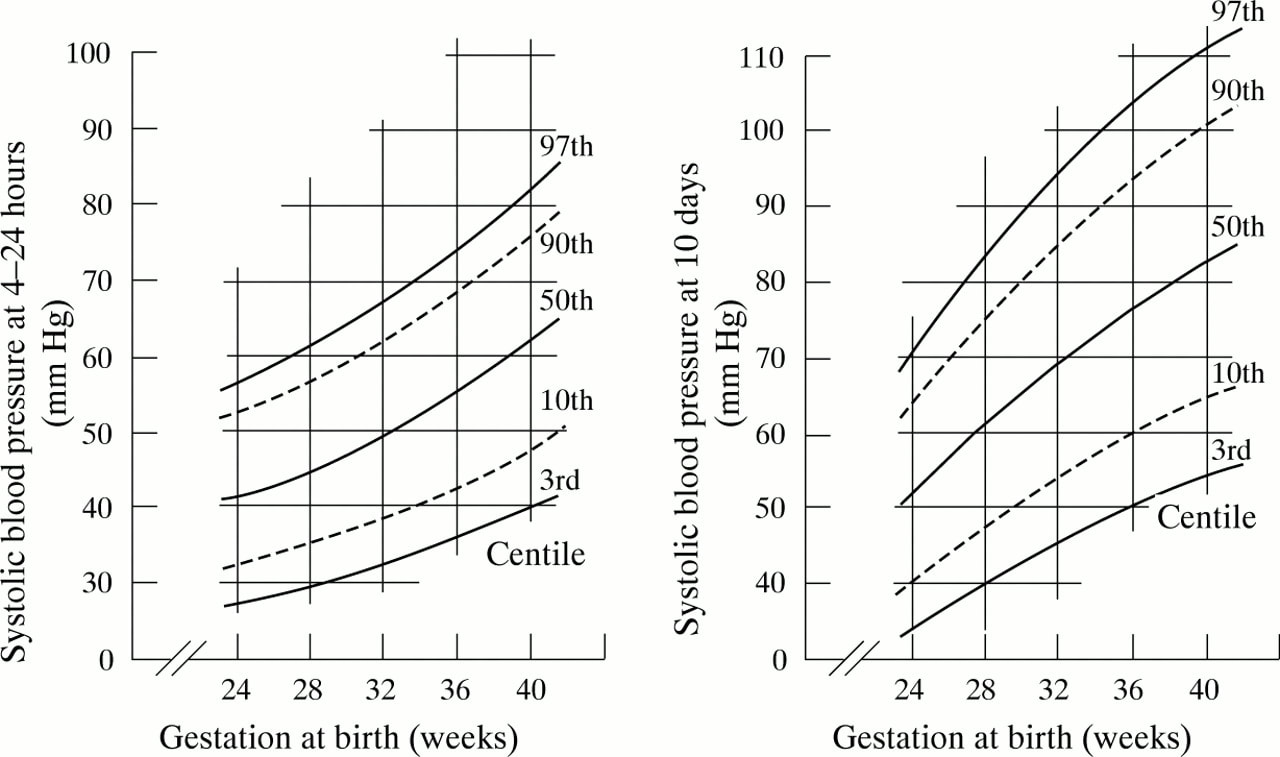
In 1990-1991 a regional study of volume expansion conducted by the NNNI in collaboration with perinatal trials unit at the National Perinatal Epidemiology Unit formed the basis of a prospective collaborative cohort of every pregnancy delivering at 22-31 weeks to a mother normally resident in the northern region and included a formal, independent neurodevelopmental assessment of all 566 survivors at the age of 2 years. To this date no other worldwide study achieved the 100% follow up data collected so carefully by Win Tin and Unni Wariyar. The volume expansion trial of 776 infants conducted in 1990-91 conclusively determined that routine use of plasma volume expansion or prophylactic use of clotting factors had no impact on rates of intra-ventricular haemorrhage (IVH). The reporting of two year outcomes made this one of the largest and most comprehensive neonatal randomised controlled trials ever conducted worldwide. The collaboration also led to the first accurate determination of 'normal physiologic' systolic blood pressure in preterm infants; to this date no other study has provided stronger data on SBP than that produced by the NNNI more than 20 years ago. It is also important to note, that whilst Newcastle has been the focus of neonatal research in the north east, Ed Hey and others were adamant that we work together as a region, and so it is appropriate to acknowledge the other neonatal units established in the 1980s including Sunderland (Sam Richmond, Majd Abu Harb), North Tees (Ian Verber, Harikumar) and Middlesbrough (Sunil Sinha, Jonathan Wyllie and Win Tin) so critical to the success of the NNNI.
The NNNI also collaborated in the OSIRIS trial of surfactant - one of the first artificial surfactant trials in preterm neonates conducted in 1991. Further studies in the late 1990s conducted as part of the northern region collaborative group were led by Dr Sean Ainsworth along with Milligan, Alan Fenton and Martin Ward Platt and showed lower mortality in infants receiving natural compared to artificial surfactants (Lancet 2000). Hey was also instrumental in planning for the internationally acclaimed studies - BOOST II that explored oxygen saturation targeting and Caffeine for Apnoea of Prematurity trials (CAP). Hey inspired generations of researchers including Malcolm Coulthard, and together Coulthard and Hey described maturation of glomerular function in the newborn in the early 1980s.
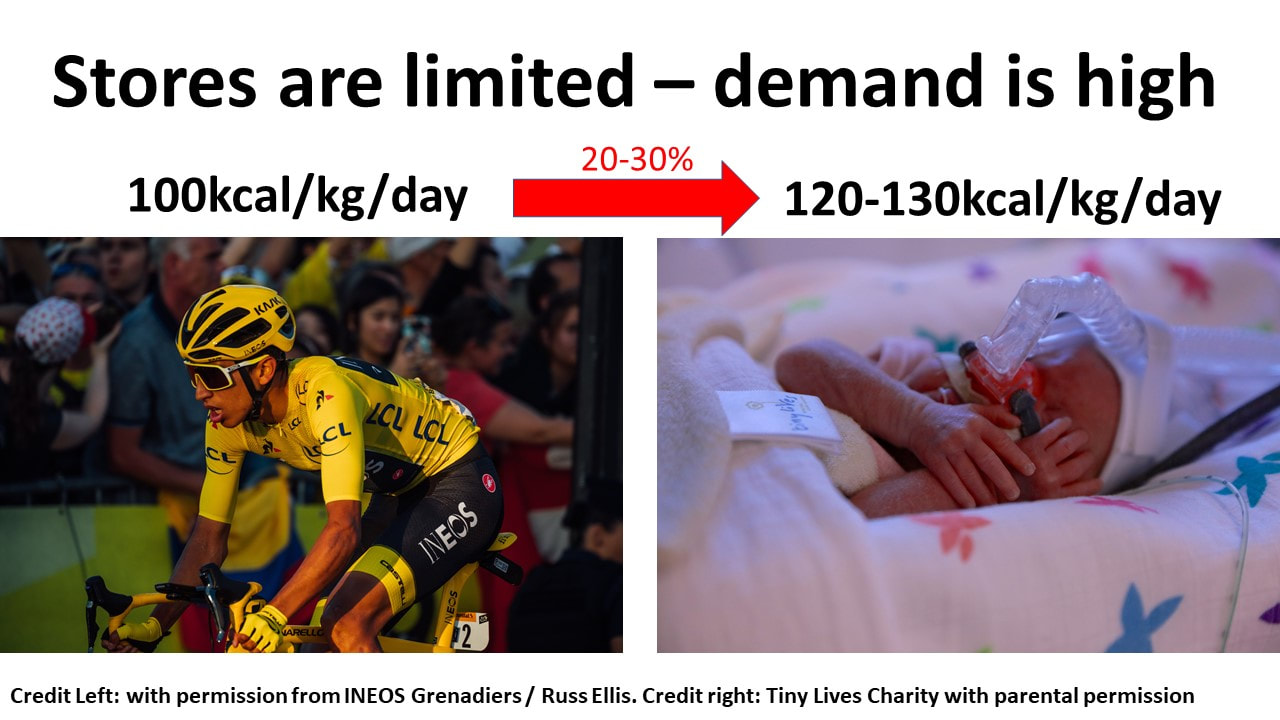
Ed Hey, Unni Wariyar and Martin Ward Platt invested in neonatal nurse training, and helped establish one of the UK's first neonatal units entirely staffed by Advanced Neonatal Nurse Practitioners (ANNPs) in Ashington and Wansbeck and published papers in relation to these key staffing developments. Dr Richard Cooke was appointed to NGH (1991-2002) to develop research into feeding of preterm infants and conducted key studies in the 1990s exploring macronutrient requirements in formula fed infants, and particularly the need for protein. These resulted in a series of highly cited papers including detailed measures of growth and body composition in the post-discharge period, and helped create cohorts of infants that have been tracked into young adulthood. Studies also explored the accuracy of linear growth measures and iron requirements. Cooke supported a number of neonatal research fellows on these projects including Jeff Perring, Ian Griffin, Kenny McCormick and Nick Embleton.
We are immensely proud of our heritage, especially in promoting, developing and supporting collaborative neonatal research. In the 2000's neonatal research in Newcastle recruited more than 1000 very preterm infants to large scale national and international collaborative trials and studies including EpiCure (outcomes for infants born less than 26 weeks), I2S2 (RCT of iodine supplementation), BOOST II UK (RCT of oxygen saturation targeting), Caffeine for Apnea of Prematurity (CAP), Speed of Increases in Feeds Trial (SIFT), Enteral Lactoferrin in Neonates (ELFIN), Mechanisms affecting the gut of preterm infants in enteral feeding trials (MAGPIE), Abnormal Doppler enteral prescription trial (ADEPT) and many more.
We stand on the shoulders of giants so that we can continue to improve care for the tiniest humans.
John Inkster, David Milligan, Martin Ward Platt (1954-2019), Edmund Hey (1934-2009), Sam Richmond (1951-2013), Janet Eyre, Unni Wariyar OBE, Alan Fenton, Jonathan Wyllie, Win Tin.
Childbirth in Newcastle-upon-Tyne: 1760s to the present day
|
It goes without saying, that changes in childbirth impact on all aspects of newborn care. Changing patterns of childbirth from 1760-1990 were beautifully summarised by Mr Derek Tacchi. Tacchi (1925-2018) was born and trained in the north east, and appointed as an obstetrician at PMMH in the 1960s, who became a scholar after retirement carefully detailing local childbirth and it his from his work that much of the following was taken.
|
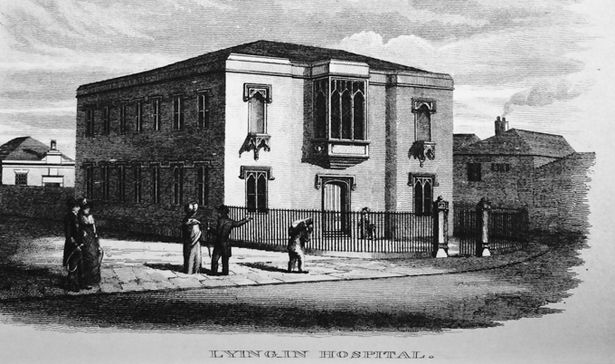
The population of Newcastle grew dramatically in the late 1700s associated with coal mining and ship building, but also improvements in public health and childbirth. The 'Lying-In hospital' opened in 1760, and charities raised money to pay for midwifery care for working class women, both in hospital and at home. The Lying-In hospital moved to a new purpose built site in New Bridge Street, central Newcastle in 1826. Most women however, continued to deliver and receive care at home. This coincided with the formal development of medical education, the most famous pupil being John Snow who later discovered the transmission of cholera and became an anaesthetist administering chloroform to Queen Victoria during childbirth. The Newcastle School of Medicine & Surgery opened in 1834 in the Hall of the Barber Surgeons Company in the Manors, midwifery was taught from 1835, and in the 1850s Newcastle amalgamated with the University of Durham. Professor Ranken Lyle was first appointed to teach midwifery in 1899 and appointed to a chair of Obstetrics & Gynaecology in 1908. Ranken Lyle was instrumental in raising funds for the Princess Mary Maternity Hospital (PMMH) opened in 1923 which remained the academic heart of neonatal research until it closed in 1993 and moved the the Royal Victoria Infirmary (RVI). In the 1930s PMMH acted as a referral centre for obstetrics, admitting women from the Tweed in the north, to the Tees in the south of what is now the northern region. Maternal death was sadly common. In 1935 from 2472 women admitted there were 77 maternal deaths due to sepsis, haemorrhage and eclampsia. This significant maternal mortality and morbidity was the driving force behind the development of the flying squad by Farquar Murray.